WISAM Attends Press Conference Announcing End to Certain Prior Authorization Requirements
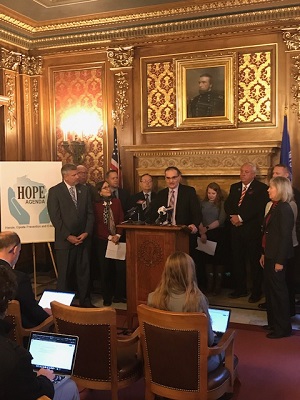
On January 21, the president of the Wisconsin Society of Addiction Medicine (WISAM), Dr. Galbis-Reig, along with representatives from Shatterproof, the Wisconsin Medical Society, and other stakeholders, attended a press conference to applaud an agreement reached by the Alliance of Health Insurers in Wisconsin and the Wisconsin Association of Health Plans to end prior authorization requirements for certain medications for addiction treatment (MAT). Under the agreement, insurers will cover at least one buprenorphine-naloxone product, methadone, injectable and oral naltrexone, and at least one form of naloxone without requiring prior authorization.
The agreement, which includes Anthem Blue Cross and Blue Shield; Children's Community Health Plan; Dean Health Plan; Network Health; MercyCare Health Plans; Quartz; Security Health Plan; United Healthcare; and WPS Health Solutions, is part of the larger HOPE Agenda, an initiative by lawmakers to address the state's opioid overdose crisis. As part of the initiative, the Wisconsin state Assembly has passed a legislative package that includes bills that would increase access to Narcan in correctional facilities and prohibit penalizing state workers for receiving MAT. The bills will now be considered by the state Senate.
Read more about the agreement here.
Click here to subscribe to The ASAM Advocate, a new, monthly ASAM e-publication, launching Thursday, February 13, 2020. The ASAM Advocate is your resource for addiction policy.
