News
Claims for Medicare’s Bundled Payment for Office-Based SUD Treatment Initiation Services Drop 37% in 2024
This blog is part of ASAM’s ‘Recovery Readout’ series, which breaks down the latest data and trends impacting addiction medicine and practice management.
Data in Focus
Over 6.8 million Medicare beneficiaries had a substance use disorder (SUD) in 2023, but nearly 80% did not receive treatment. Of those diagnosed with a SUD, just about 20% (1.2 million) received any treatment at all.
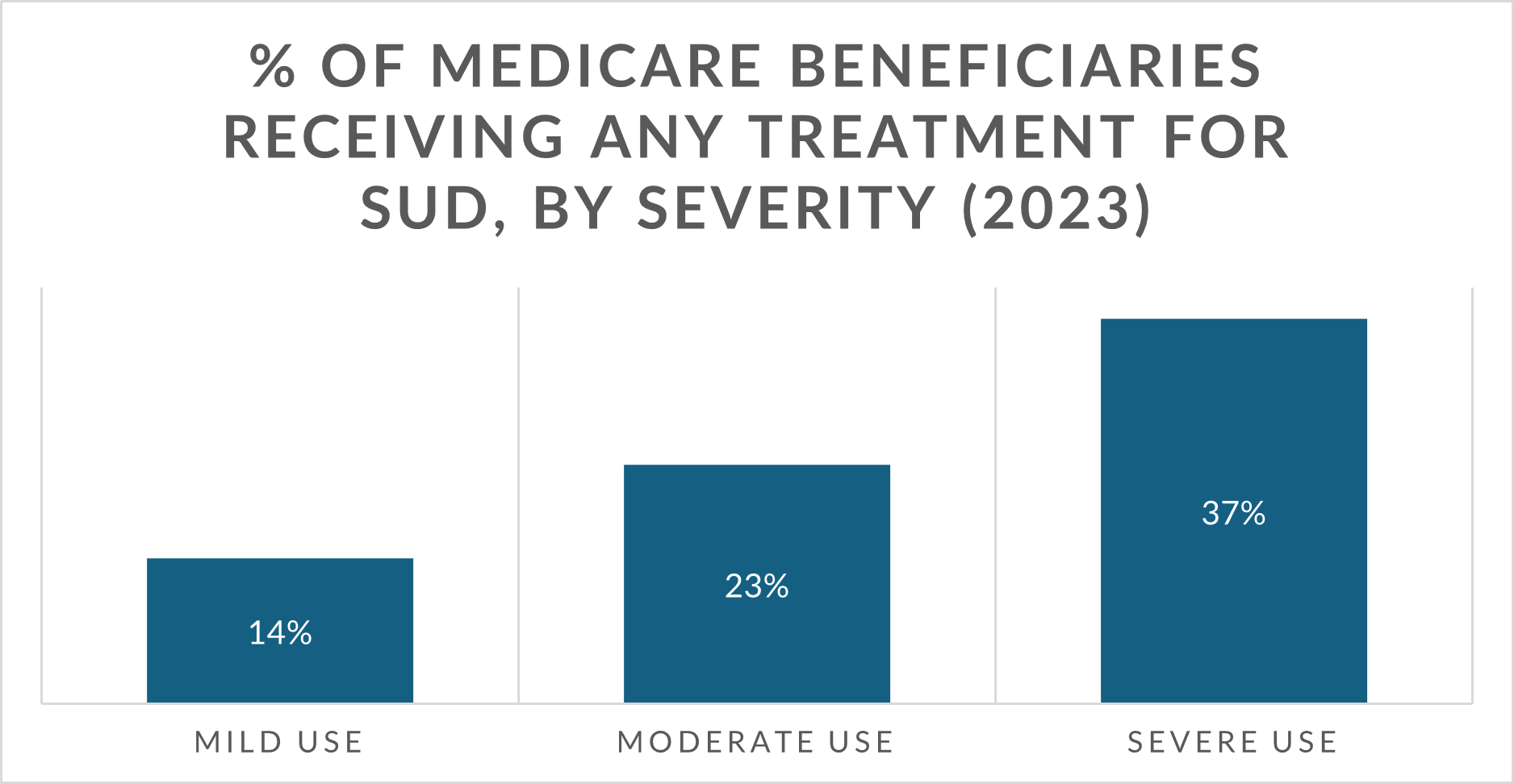
Looking at those diagnosed with a mild, moderate, or severe SUD, the lowest percentage of beneficiaries receiving any treatment were those with a mild use disorder, despite this category being the highest percentage of Medicare beneficiaries.
Outpatient treatment was the most common treatment method (75%) for Medicare beneficiaries, with most beneficiaries (53%) having a mild use disorder, suggesting it’s well-suited for milder cases.
Source: ASAM analysis of National Survey on Drug Use and Health, 2023
Data Disconnect
However, provider billing practices don’t match outpatient treatment rates. Medicare claims data show only about 1,800 total claims for bundled payment for initial office-based treatment in 2023 – the service championed by CMS to treat SUD in office-based/non-OTP settings. That figure fell to just over 1,100 claims in 2024 – a roughly 37% drop.
- Nearly 68% of those SUD treatment initiation claims were from nurse practitioners, physician assistants, internists, and family physicians. Only 3% were rendered by addiction specialist physicians (ASPs).
Compare those figures to opioid treatment program (OTP) claims through September 2024 showing that almost 1,800 Medicare beneficiaries visited OTPs for opioid use disorder (OUD) treatment with buprenorphine or naltrexone, higher than the SUD treatment initiation services in each year from 2022-2024. Caveat: non-OTPs cannot dispense methadone and OTPs cannot bill Medicare for non-OUD services.
For context, the office-based SUD treatment and OTP numbers are far below the almost half a million beneficiaries that reported receiving outpatient treatment for SUD in 2023, according to SAMHSA.
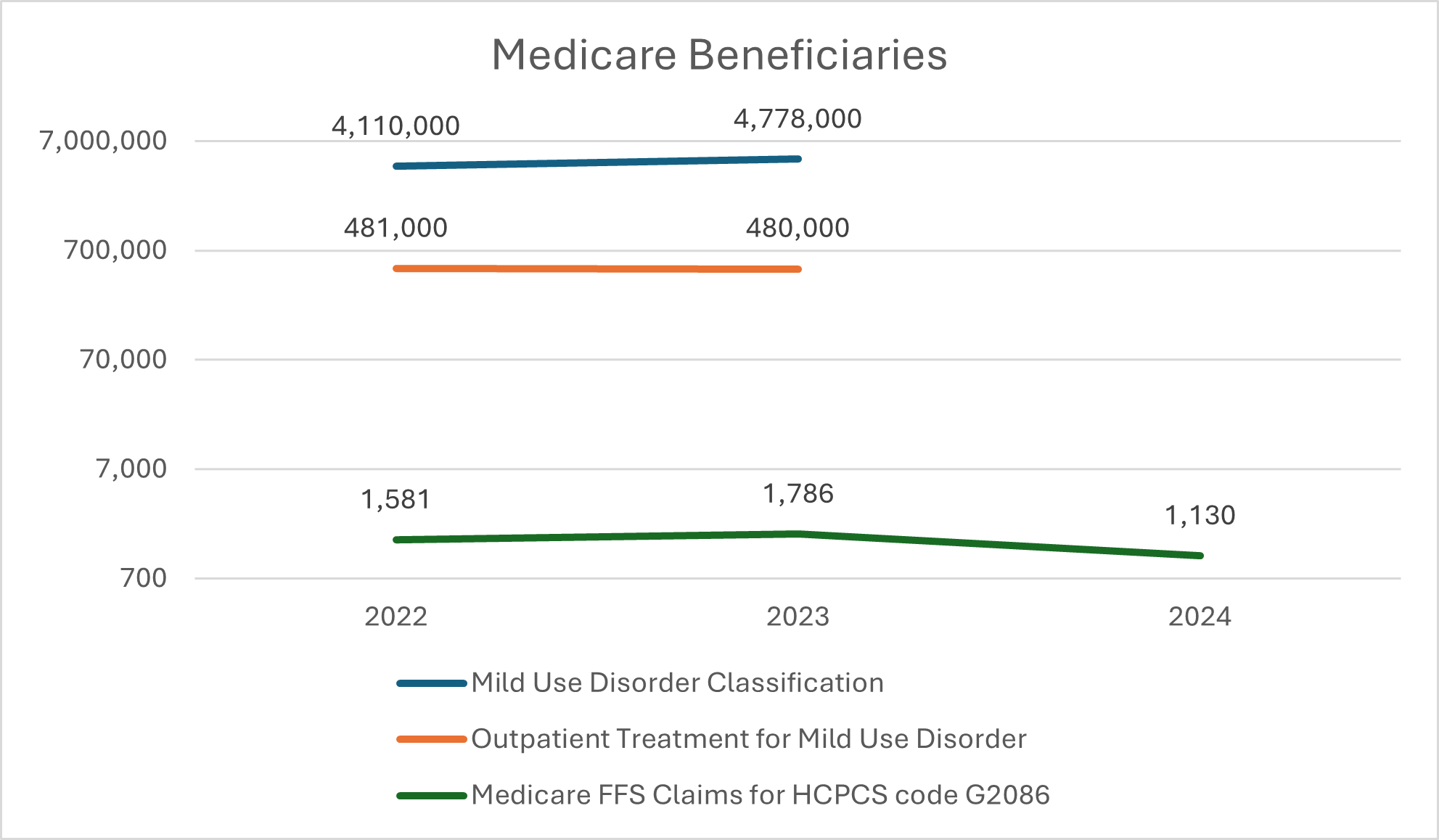
Source: ASAM analysis of Medicare Fee-for Service utilization data, 2022-2024 & ASAM analysis of National Survey on Drug Use and Health, 2022-2023
Note: 2024 NSDUH crosstabs were not available for analysis at the time of publication.
Zoom Out
The Medicare data do not appear to capture thousands of Medicare beneficiaries reporting outpatient treatment, but they do offer some clues that may inform future rule and policymaking, including:
Medicare providers appear to be using other HCPCS codes to report office-based SUD treatment initiation, given the significant disparity between beneficiaries reporting they received outpatient treatment and the claims numbers;
The discrepancy suggests that clinicians are either unaware of the bundled payment office-based codes, or they believe other codes are more suited to report their services. A report from the HHS Inspector General recommended that CMS increase its education outreach about covered SUD treatment services;
Unlike OTP codes that describe medical management and psychosocial support services, Medicare’s SUD treatment initiation codes describe the psychosocial components of treatment, not the medical management services described by E/M codes that many clinicians may be billing;
At the same time, the higher utilization of the office-based treatment initiation codes among nurse practitioners, interventional pain management specialists, family medicine physicians, and emergency medicine doctors suggest that these codes may be valued just high enough to incentivize these clinicians to take on new patients who may have an acuity level these clinicians are comfortable managing, possibly recouping payment far higher than they would under regular E/M codes;
In contrast, claims data on E/M visits billed by ASPs suggest they see new patients who present with greater medical acuity. 80% of E/M visits for new patients billed by ASPs in 2024 were for visits requiring moderate/high level clinical decision-making, compared to 43% for PAs/NPs, 58% for family physicians, and 76% for internists. This suggests that ASPs see patients with more moderate to severe SUD cases and that the value of the SUD initiation code may be lower than their actual spend per patient;
It is also possible that patients visiting outpatient clinics are stable with medical management and do not want the additional psychosocial supports, therefore foregoing the need to bill for the treatment initiation services that include the psychosocial supports;
Many clinicians providing outpatient care coordination and psychotherapy for SUD may be billing the services described by the code as standalone rather than bundled services;
In fact, there were over 32,000 claims for initial psychiatric collaborative management services, and 1.8 million for psychotherapy in 2024 (the services described by Medicare’s codes), well over the number of claims for Medicare’s bundled payments for office-based treatment codes; and
Finally, compare payment rates for treatment with buprenorphine in non-OTP office-based settings with the same treatment in OTPs: >$900 for 4 weeks of treatment in an OTP vs. <$500 for the same treatment in a non-OTP. Medicare’s payment incentives could be misaligned.
Yet, this is only part of the picture since more than half of Medicare beneficiaries are in Advantage plans that do not make similar data readily available.
The Impact
Despite the data showing a substantial gap between the number of Medicare beneficiaries with a SUD vs. those receiving treatment, the fee-for-service claims data offers a limited window into how Medicare-participating clinicians are addressing SUD.
CMS stated in the 2020 Medicare Physician Final Rule that its new office-based SUD treatment codes were aimed at increasing the use of counseling and care coordination services and expected to be mostly utilized by ASPs. Claims data suggest, however, that these codes have not met their intended purpose as their utilization plummets, ASPs are among the lowest utilizers, and millions of beneficiaries are not getting treatment.
Takeaways
CMS should review Medicare’s office-based SUD treatment codes to ensure they are meeting their intended purpose and consider several actions, including:
Providing more robust clinician education and outreach about the services covered by Medicare for the treatment of SUDs;
Making significant coding modifications to the office-based SUD treatment set that account for medical management in cases where a billing practitioner is providing comprehensive biopsychosocial initiation services directly or through supervision, similar to the existing OTP payment structure. ASAM has outlined the Patient-Centered Opioid Addiction Treatment (P-COAT) model which describes three types of treatment initiation payment structures: (1) treatment supervision and medical management by a non-ASP, (2) treatment supervision and medical management by an ASP, OR (3) comprehensive medical management and psychosocial services. Additional coding granularity would also mirror the OTP code set which is much more detailed, structured, and financially sustainable;
Adding several codes limited to OTPs as services eligible for billing by non-OTP practices to the extent those services are not duplicative of existing services described by the initiation codes;
Providing additional public-facing data about the use of E/M services in Medicare to provide SUD treatment to understand the extent to which Medicare patients receive medical services to address SUD.
Stories Behind the Stat
Go Deeper
For more information on services to address SUD covered by Medicare, click here.
View a data brief from HHS OIG, Not All Medicare Enrollees Are Continuing Treatment for Opioid Use Disorder, to learn about HHS’ recommendations to improve treatment engagement and billing practices.
